Atrioventricular Valve Dysplasia in Dogs: 2025 Vet Guide 🩺🐶
In this article
Atrioventricular Valve Dysplasia in Dogs: 2025 Vet Guide 🩺🐶
By Dr. Duncan Houston BVSc
Hi, I’m Dr Duncan Houston, BVSc, veterinarian and founder of Ask A Vet. In this comprehensive 2025 guide, we'll explore atrioventricular (AV) valve dysplasia in dogs—a congenital defect affecting the mitral or tricuspid valves. We’ll cover causes, signs, advanced diagnostics, treatment, prognosis, and how telehealth enhances care.
1. 🫀 What is AV Valve Dysplasia?
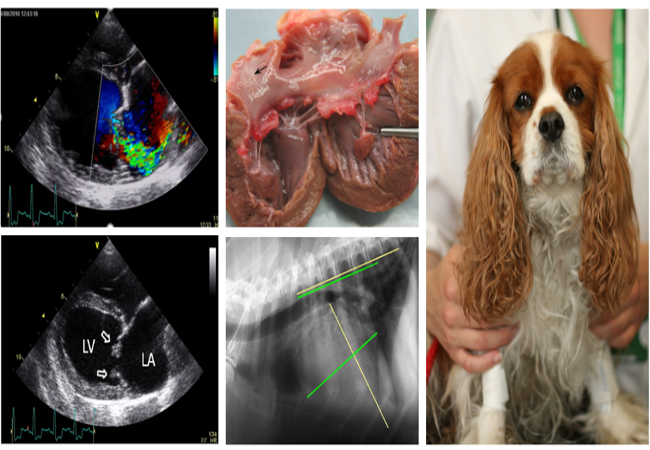
AV valve dysplasia is a congenital malformation of the mitral or tricuspid valve complex, including leaflet thickening, shortened or fused chordae, abnormal papillary muscles, or malattachment—resulting in regurgitation and/or stenosis. The tricuspid form affects right-side flow; mitral form impairs left-side flow.
2. 🧬 Causes & Breed Predisposition
- Congenital origin: Present at birth, often inherited.
- Breed risk: Mitral dysplasia commonly seen in Bull Terriers, Great Danes, Rottweilers, Golden Retrievers, Dachshunds, Labs, German Shepherds, Mastiffs, and Dalmatians.
- Tricuspid dysplasia: Predominant in Labs, German Shepherds, Irish Setters, Great Danes, Old English Sheepdogs, and Boxers.
- Coexisting defects: May include subaortic stenosis, pulmonic stenosis, and septal defects.
3. ⚠️ Clinical Signs & When They Appear
- Signs often emerge in dogs <2 years old; mild cases may be silent for years.
- Mitral dysplasia signs: systolic murmur at apex, atrial enlargement, exercise intolerance, coughing, dyspnea, pale/bluish gums.
- Tricuspid dysplasia signs: right-sided murmur, jugular distension, ascites, leg edema, right-sided CHF.
- Arrhythmias (supraventricular or atrial fibrillation) and syncope may occur.
4. 🎧 Detecting Murmurs & Diagnostic Evaluation
Auscultation reveals holosystolic murmurs; thrill may be palpable. Severity depends on leak size and flow.
Diagnostics Include:
- Chest X-rays: chamber enlargement, pulmonary edema/effusion signs.
- ECG/Holter: arrhythmias, atrial enlargement, conduction delays.
- Echocardiography + Doppler: definitive—visualizes leaflet abnormalities, chordae, papillary muscles, regurgitation jets, pressure/volume changes.
- Bloodwork: baseline, biomarker assessment (e.g., NT-proBNP).
- Further imaging and genetic testing if planning breeding decisions.
5. 🛠 Grading Severity
- Mild: minimal regurgitation, no chamber dilation, asymptomatic.
- Moderate: chamber enlargement, occasional exercise intolerance or arrhythmia.
- Severe: overt CHF, ascites, pulmonary edema, syncope, arrhythmias, possible premature death.
6. 💊 Treatment Strategies
a. Medical Management
- No CHF: asymptomatic monitoring only.
- Developing CHF: diuretics (furosemide), ACE inhibitors (enalapril, benazepril), pimobendan, venodilators, low-sodium diet.
- Arrhythmia control: anti-arrhythmics (e.g., atenolol, sotalol, mexiletine, procainamide).
- Restrict exercise and stress.
b. Surgical & Interventional Options
- Open-heart valve repair/replacement has been attempted but is limited by cost, availability, and variable outcomes.
- Emerging interventions (e.g. chordal repair, commissurotomy) could become more available.
7. 📈 Prognosis & Survival
- Mild cases: often live normal lifespans with periodic monitoring.
- Moderate to severe without CHF: may survive months to years with treatment.
- CHF onset: long-term prognosis poor; median survival ~1–2 years for severe mitral dysplasia, ~6 months post-CHF onset; TVD median survival ~7.5 years without CHF, ~6 months with CHF.
- Early detection and therapy slow progression and enhance quality of life.
8. 🏡 Home Care & Monitoring
- Track resting respiratory rate (>30–35/min) and effort.
- Log exercise tolerance, coughing, collapse, ascites, or edema.
- Maintain low low-sodium diet and follow the medication schedule via reminders.
- Recheck echo/ECG every 6–12 months, or sooner with worsened signs.
9. 🌐 2025 Telehealth & Innovation
- Wearable stethoscope/ECG patches: remote screening for murmurs and arrhythmias.
- AI auscultation and echo analysis: detects valve defects, jet severity, and chamber enlargement.
- Echo/ECG upload: remote review by Ask A Vet specialists.
- App reminders/alerts: meds, vitals, respiratory signs.
- Virtual consults: for medication adjustment, surgery evaluation, or severity staging.
- Telemonitoring CHF episodes: alerts for early diuretic needs.
10. 🐕 Breeds & Life Stage Considerations
- Puppies/young dogs: often symptomatic early; early diagnosis crucial.
- Large breeds: Great Danes, Labs, and GSDs are at increased risk.
- Genetic screening: avoid breeding affected dogs due to hereditary risk.
11. 💬 FAQs
- Will correcting the valve fix it?
- Valve surgery has been tried but isn't routinely available; medical care remains the mainstay.
- Can my dog live a good life?
- Yes—mild cases usually thrive; moderate/severe cases need monitoring & CHF management.
- Is this preventable?
- No, it's congenital—but early detection and avoiding breeding are key.
- How often should we see the vet?
- Every 6–12 months if stable; every 2–4 months once CHF begins.
12. ❤️ Ask A Vet Telehealth Support
- Remote echo & ECG uploads for specialist review
- AI murmur detection and valve assessment
- Medication reminders and dose-tracking tools
- Virtual follow-ups to adjust therapy or discuss surgery
- Emergency alerts for breathing difficulty or collapse
Download our app to connect your dog’s valve care with expert oversight—anytime, anywhere. 🐾❤️
13. 🔚 Final Summary
AV valve dysplasia is a congenital disorder affecting mitral or tricuspid valves, leading to regurgitation, chamber overload, arrhythmias, and heart failure. Diagnosis relies on echocardiography and ECG. Treatment includes CHF medications and arrhythmia control; surgery is rarely available. Prognosis depends on severity—mildly affected dogs can live normally, while severe cases need ongoing management. In 2025, telehealth tools like wearables, AI-assisted diagnostics, and virtual care will enhance early detection, monitoring, and tailored treatment. Partnering with Ask A Vet and your primary vet ensures optimal support throughout your dog's life.
— Dr Duncan Houston, BVSc






