Hemangiosarcoma in Dogs: 2025 Vet Guide on Diagnosis, Treatment & Hope 🩺🐶
In this article
Hemangiosarcoma in Dogs: 2025 Vet Guide on Diagnosis, Treatment & Hope 🩺🐶
By Dr. Duncan Houston BVSc
Hi there! I’m Dr Duncan Houston, BVSc, veterinarian and founder of Ask A Vet. Hemangiosarcoma (HSA) is a common yet aggressive cancer in dogs, arising from the blood vessel lining. This 2025 guide covers risk factors, signs, diagnostics, treatments—including new vaccine options—and how telehealth can support diagnosis and management every step of the way. Let’s dive deep to equip you with knowledge and hope. ❤️🐾
1. What Is Hemangiosarcoma?
Hemangiosarcoma is a malignant tumor of vascular endothelium (cells lining blood vessels), highly invasive in dogs. It frequently arises in the spleen, heart (right atrium/auricle), liver, or skin. It accounts for 5–7% of canine cancers.
2. 🧬 Risk Factors & Predisposed Breeds
- Occurs most often in older, large-breed dogs (German Shepherds, Golden Retrievers, Labrador Retrievers, Boxers).
- It can appear in younger dogs, but less common.
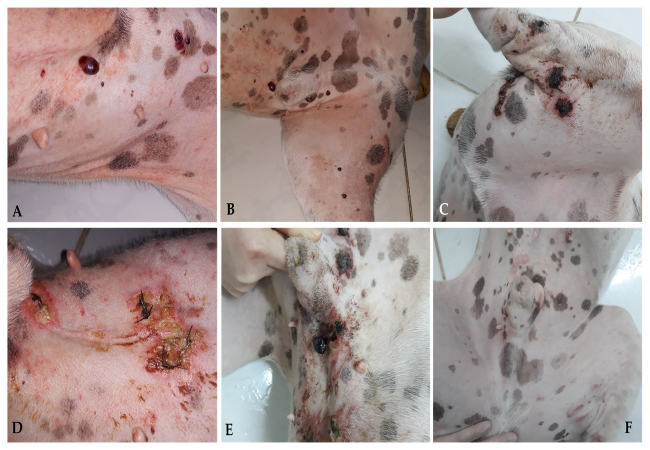
- Dermal forms linked to sun exposure in light-coated, thin-haired dogs like Dalmatians, Greyhounds.
3. ⚠️ Why It’s Dangerous
HSA tumors are fragile and tend to rupture, causing life-threatening hemorrhage into the abdomen (hemoabdomen) or pericardial sac (cardiac tamponade). They also metastasize quickly—common sites include the lungs, liver, omentum, and brain.
4. 🩹 Signs & Emergency Presentation
- Often asymptomatic until sudden collapse, pale gums, lethargy, rapid breathing due to internal bleeding.
- Cardiac forms may present with muffled heart sounds, arrhythmias, right-sided effusion, and exercise intolerance.
- Skin lesions appear as red/blue masses that bleed easily, sometimes curable.
5. 🧪 Diagnostic Pathway
- Physical exam & history: Collapse, distended abdomen, muffled heart sounds.
- Bloodwork: CBC (anemia, low platelets, DIC signs), chemistry, coagulopathy markers.
-
Imaging:
- Abdominal ultrasound: Splenic or liver masses, effusion
- Chest X‑rays / CT: Look for metastasis
- Echocardiography: Detect right atrial masses or effusions.
- Pericardiocentesis: Relief and sample cytology if tamponade suspected.
- Definitive diagnosis: Requires biopsy or surgical histopathology.
6. ✂️ Treatment Options & Expected Outcomes
a. Splenic HSA
- Splenectomy: Removal of the affected spleen—crucial first step. Recurrence risk remains without further therapy.
- Chemotherapy: Doxorubicin-based protocols post-splenectomy can extend survival to an average of 5–6 months.
- Prognosis: Splenectomy alone ≈1–3 months; chemo adds ~2–4 more months on average.
b. Cardiac HSA
- Pericardiocentesis: Immediate drainage can stabilize, but the tumor remains.
- Continuous effusion: Surgical pericardiectomy and experimental debulking in select cases.
- Chemotherapy: May delay progression, survival estimates ≈4–6 months.
c. Cutaneous / Subcutaneous HSA
- Surgical excision: Can be curative if margins are clean.
- Adjuvant therapy: Chemo or radiation is used if aggressive. Prognosis is good when superficial.
d. Experimental & Emerging Therapies
- Cancer Vaccine: Calviri's off-the-shelf immunotherapy vaccine targeting early-stage HSA is in trial (SOCH trial, FDA 2024).
- Personalized immunotherapy: Tumor DNA profiling guiding treatments like tyrosine kinase inhibitors (TKIs).
- Mushroom extract adjuncts: Coriolus versicolor studied—offers mixed results; not standard.
7. 📈 Prognosis by Form
- Splenic HSA: ~1‑3 months post-splenectomy alone; 5‑6 months with chemo.
- Cardiac HSA: ~4–6 months survival with combined treatment, often shorter.
- Cutaneous HSA: Excellent prognosis with complete removal—often cured.
- Vaccine adjunct: Goal is to improve survival; trials underway.
8. 🏡 Home Care & Monitoring
- Observe for signs of bleeding: pale gums, weakness, sudden lethargy.
- Record appetite, energy, breathing, and abdominal size.
- Ensure rest post-surgery/chemotherapy; follow vet’s instructions on activity.
- Track vaccine or chemo side effects: appetite loss, vomiting, weakness.
- Schedule follow-up scans (echocardiogram, ultrasound) and blood tests every 3‑6 months.
9. 🌐 Telehealth & Care in 2025
- Ask A Vet app: Upload emergency symptoms, scans, and ECGs immediately.
- Remote imaging review: Specialists analyze echo/ultrasound for early tumor detection.
- Medication & appointment reminders: Keeps chemo, imaging, and recovery schedules on track.
- AI early alerts: Tracks vitals, behavior changes, and prompts vet consultations.
- Virtual consults: For ongoing treatment, emergency signs, and home care optimization.
10. 💬 FAQs
- Can hemangiosarcoma be cured?
- Cutaneous HSA can often be cured. Splenic and cardiac forms aren’t curable but treatments may extend life with good quality.
- When should I suspect HSA?
- Sudden collapse, abdominal swelling, rapid breathing, pale gums—especially in high‑risk breeds.
- Are vaccines worth it?
- Still investigational—early results hopeful, but not yet standard. Clinical trials are open at veterinary oncology centers.
- How do I choose a treatment plan?
- Decisions are based on tumor location, clinical signs, the owner's goals, and the feasibility of surgery and chemo.
11. ❤️ Ask A Vet Telehealth Support
- Emergency check-ins: Sudden collapse or bleeding concerns.
- Scan reviews: Remote echo/ultrasound interpretation by specialists.
- Treatment reminders: Chemo, post‑op, vaccine visits.
- Side effect monitoring: For appetite, hydration, and energy.
- Virtual care plans: Customized care between in‑clinic visits.
Download the Ask A Vet app to keep your dog supported—during treatment, recovery, and breakthroughs. 🐾❤️
12. 🔚 Final Summary
Hemangiosarcoma is fast-moving and often hidden until a crisis. Yet with prompt recognition, surgical treatment, chemotherapy, and emerging immunotherapies—including promising vaccine trials—dogs can live months longer with comfort. Telehealth tools like remote imaging review, AI alerts, and specialist support amplify your vet's power at home. Not all is lost; together, we stand strong in the face of this challenge—every heartbeat matters.
— Dr Duncan Houston, BVSc






