Vet’s 2025 Guide to Eosinophilic Pneumonia in Dogs 🐶 Immune-Mediated Lung Inflammation🩺
In this article
Vet’s 2025 Guide to Eosinophilic Pneumonia in Dogs 🐶 Immune-Mediated Lung Inflammation🩺
By Dr. Duncan Houston BVSc
💡 Introduction
Eosinophilic pneumonia is a form of allergic or immune‑mediated pneumonia characterized by infiltration of eosinophils—specialized white blood cells—in the lung tissues and airways. It is uncommon, but important to recognize, as it often responds well to treatment once correctly diagnosed.
1. What Is Eosinophilic Pneumonia?
This condition involves eosinophils accumulating in the alveoli and bronchial walls, along with fluid, resulting in impaired gas exchange and respiratory distress, but without bacterial infection as the primary cause.
2. Who Is Affected?
- Affects dogs of any age or breed; younger dogs may be more common.
- No clear breed predisposition—but outdoor dogs exposed to allergens, dust, and parasites are at higher risk.
- Owners in dusty, moldy, or high-pollen environments should be especially watchful.
3. Clinical Signs & Symptoms ⚠️
- Cough: often chronic, may be dry or productive.
- Dyspnea & tachypnea: labored breathing, exercise intolerance, lethargy.
- Fever, weight loss: may suggest systemic involvement.
- Occasional nasal discharge or sneezing.
4. Triggers & Underlying Causes 🧩
- Parasitic lung infections, such as heartworm, lung flukes.
- Allergens: pollen, mold, dust mites, airborne irritants.
- Idiopathic or autoimmune: no trigger identified.
- Medication or toxin exposures: environmental or drug-related.
5. Diagnosis in 2025 🧪
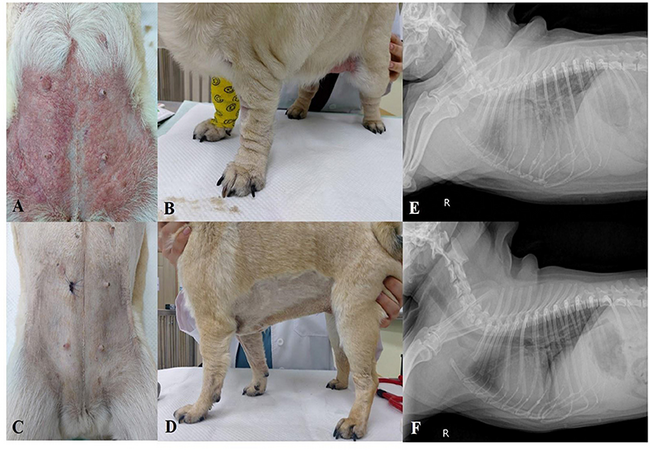
5.1 Physical Exam & Imaging
- Auscultation: crackles, wheezes, or harsh bronchial sounds.
- Thoracic x‑rays: diffuse bronchointerstitial or alveolar patterns, patchy infiltrates.
- Ultrasound: “lung rockets” may be seen in parenchymal disease.
5.2 Bronchoalveolar Lavage (BAL)
The gold-standard diagnostic step: collecting lower airway fluid and examining it under a microscope. >50% eosinophils confirms the condition . BAL also helps rule out parasites, bacteria, and fungi via cytology or culture .
5.3 Bloodwork & Other Tests
- CBC may show peripheral eosinophilia in ~50% of cases.
- Rule out heartworm, fungal, or parasitic infections via serology or fecal exam.
- Biopsies are rarely needed unless the diagnosis is unclear.
6. Treatment & Management (2025) ❤️
6.1 Corticosteroids
- Prednisone/prednisolone oral anti-inflammatory therapy: typical dose 1 mg/kg 12‑hourly for 3–4 weeks, taper over months.
- Inhaled steroids (e.g., fluticasone via spacer) reduce systemic side effects.
6.2 Addressing Underlying Triggers
- Parasite treatment—heartworm or lung flukes.
- Allergen reduction—air filtration, hypoallergenic environments.
- Avoid toxins/chemicals in the environment.
6.3 Supportive Care
- Oxygen therapy for severe dyspnea.
- Antibiotics only if a secondary infection is present.
- Nebulization and coupage may aid mucus clearance.
7. Prognosis & Follow-up Care
- Many dogs respond dramatically to corticosteroids within days.
- Some require lifelong low-dose therapy—fluticasone via inhaler helps minimize systemic impact.
- Relapse can occur—restart treatment and taper slowly.
- Prognosis is generally good with proper management.
8. Home Monitoring & Ask A Vet Support 🏡
- Track cough frequency, breathing rate, exercise tolerance, and alert team if worsening.
- Photo/video uploads showing breathing patterns help remote evaluation.
- Medication reminders, taper reminders, refill alerts.
- Environmental checklists to reduce allergens and dust exposure.
- Support in case of relapse or infection flare-ups.
🔍 Key Takeaways
- Eosinophilic pneumonia is an immune/allergic lung disease characterized by eosinophil accumulation.
- Symptoms include persistent cough, difficulty breathing, and exercise intolerance.
- An accurate diagnosis requires BAL with eosinophil cytology.
- Corticosteroid therapy is highly effective, often life-changing.
- Addressing triggers like parasites and allergens improves outcomes.
- Ask A Vet connects home monitoring, treatment reminders, and breathing support.
🩺 Conclusion ❤️
Eosinophilic pneumonia may be uncommon, but it often hides behind chronic cough or intermittent breathing issues. In 2025, with precise diagnostics and effective corticosteroid treatment, most dogs experience dramatic improvement. Addressing underlying triggers and utilizing tools like Ask A Vet ensures long-term control and optimal lung health for your pup. 🐶✨
Dr Duncan Houston BVSc – guiding compassionate, science-based respiratory care for dogs.
Visit AskAVet.com and download the Ask A Vet app for treatment tracking, breathing alerts, environment checklists, and dedicated support through respiratory episodes. ❤️






