Veterinary Guide to Canine Hypoxemia 2025 🐶💨🩺
In this article
Veterinary Guide to Canine Hypoxemia 2025 🐶💨🩺
By Dr. Duncan Houston BVSc
🧬 What Is Hypoxemia?
Hypoxemia refers to low arterial blood oxygen (PaO₂ < 80 mm Hg, SpO₂ < 90 %), indicative of serious oxygen delivery issues to tissues.
👥 Who's at Risk?
- Dogs with respiratory disease: pneumonia, pulmonary edema, fibrosis, airway obstruction.
- Cardiac patients: heart failure, congenital shunts causing V/Q mismatch.
- Neuromuscular or CNS disease: causing hypoventilation.
- Anemia or airway trauma may also precipitate hypoxemia.
⚠️ Clinical Signs
- Tachypnea, dyspnea, open-mouth breathing.
- Coughing, gagging, cyanotic mucous membranes.
- Tachycardia, collapse, weakness or seizures.
- Noisy breathing—stridor, wheezes, crackles.
🔍 Diagnostics & Evaluation
- Pulse oximetry + ABG: confirm PaO₂/SpO₂ and check PaCO₂ to identify underlying pathology.
- Thoracic imaging: chest X-ray or ultrasound to assess lung fields, pleural effusion, edema, pneumonia.
- Cardiac evaluation: echocardiography, ECG, blood pressure—identify structural or functional heart disease.
- Complete blood work: CBC, biochemistry, PCV to rule out anemia, systemic disease, and monitor perfusion.
- Neurologic or airway assessment: evaluate for hypoventilation, upper airway obstruction, CT/MRI when indicated.
🛠️ Treatment Strategies
1. Immediate Oxygen Support
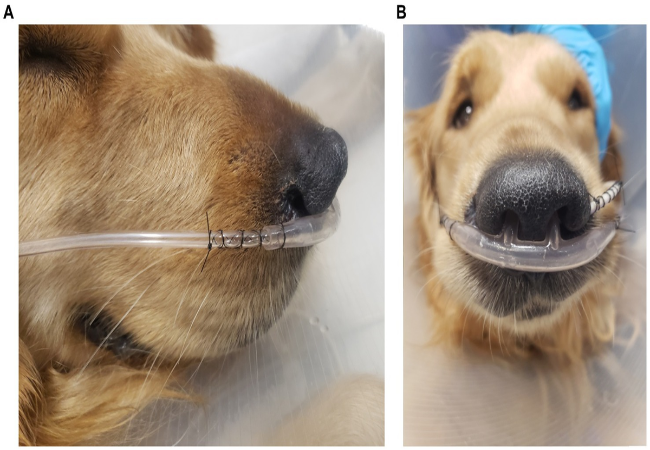
- Provide supplemental oxygen via mask, nasal prongs, or oxygen cage.
- High-flow nasal cannula (HFNC): offers better PaO₂ and lowers respiratory effort than conventional oxygen therapy.
- Administer IV fluids to optimize perfusion and oxygen delivery.
2. Address Underlying Disease
- Pneumonia: antibiotics, nebulization, chest physiotherapy.
- Pleural effusion: thoracocentesis and targeted therapy.
- Heart failure: diuretics, ACE inhibitors, oxygenation support.
- Hypoventilation: reversal of sedatives, ventilation support.
- Anemia: transfusion if needed.
3. Monitoring & Advanced Support
- Continuous SpO₂, ETCO₂, and ECG monitoring.
- Repeat ABG and chest imaging every 6–12 hours.
- Consider ICU-level support: mechanical ventilation for severe cases.
4. Long-Term Management
- Oxygen supplementation at home during bouts of disease.
- Manage chronic cardiac or respiratory conditions.
- Regular follow-ups with pulse ox and chest imaging as needed.
📈 Prognosis
- Dependent on the underlying cause: prompt treatment often leads to full recovery.
- Severe respiratory disease or cardiac failure may require long-term care.
- Hypoventilation from neurologic damage may carry guarded prognosis.
📱 Ask A Vet Telehealth Support
- 📸 Share photos/videos of breathing effort and monitor tracings remotely.
- 🔔 Get guided instructions on oxygen setup, HFNC use, and fluid therapy.
- 🩺 Virtual checks on vitals, respiratory rate, and recovery progress.
🎓 Case Spotlight: “Luna” the Frenchie
Luna, a 6-year-old French Bulldog, presented with severe dyspnea and cyanosis. SpO₂ was 82 %, ABG confirmed PaO₂ 60 mm Hg. Chest X-ray showed pneumonia; elevated cardiac markers ruled out failure. She was placed on HFNC, started on IV antibiotics and fluids. Ask A Vet supported remote monitoring, and guided follow-ups. Luna’s SpO₂ normalized within 48 hours, and she recovered fully within a week 🐾.
🔚 Key Takeaways
- Hypoxemia is life-threatening—watch for cyanosis, dyspnea, and collapse.
- Diagnosis relies on ABG, SpO₂, imaging, and blood work.
- Treatment must include supplemental oxygen (HFNC when possible), fluids, and condition-specific care.
- Continuous monitoring is crucial in early stages and recovery.
- Ask A Vet telehealth provides remote support, oxygen guidance, monitoring, and equipment delivery for optimal outcomes 📲🐕
Dr Duncan Houston BVSc, founder of Ask A Vet. Download the Ask A Vet app to access expert telehealth for hypoxemia—get guided oxygen therapy, remote vital checks, medication coordination, and equipment delivery to support breathing emergencies 🐶📲






