Veterinary Guide to Canine Strongyloidiasis 2025 🩺🐶
In this article
Veterinary Guide to Canine Strongyloidiasis 2025 🩺🐶
By Dr. Duncan Houston BVSc
🧬 What Is Strongyloidiasis?
Strongyloidiasis is caused by the small nematode Strongyloides stercoralis (also known as S. canis in dogs). These parasites inhabit the small intestine lining, and, unique among nematodes, females reproduce by parthenogenesis. Infection can be asymptomatic or cause intestinal and pulmonary disease.
🌍 Lifecycle & Zoonotic Risk
The life cycle alternates between parasitic and free-living stages. Infective third-stage larvae (L3) penetrate skin or are ingested, migrate via the lungs to the intestine, and mature into females that produce rhabditiform L1 larvae shed in feces. Autoinfection (internal reinfection) can perpetuate infection indefinitely.
Dogs are potential zoonotic reservoirs; genetic studies support cross-infection between dogs and humans.
👥 Who’s Affected?
- Young puppies and immunocompromised dogs are most at risk of clinical disease.
- Seen worldwide, especially in warm, humid, and unsanitary environments.
- Imported or traveling dogs may introduce infection to non-endemic regions.
⚠️ Clinical Signs
- Diarrhea (often intermittent, mucoid, or blood‑flecked), weight loss, and malabsorption.
- Coughing, respiratory distress—larval lung migration (“Loeffler’s syndrome”).
- Skin dermatitis or larva currens (rapid rash) at larval entry sites.
- In severe or hyperinfection cases: stunting, anemia, dehydration, systemic signs; high mortality in immunocompromised dogs.
🔍 Diagnosis
- History & exam: Note risk factors—poor hygiene, kennels, travel, and immune status.
- Baermann fecal test: Gold standard for detecting fresh larvae in feces.
- Multiple samples: Required due to intermittent larval shedding.
- Cytology of sputum or skin scrapings: May reveal migrating larvae in respiratory or dermatologic cases.
- Serologic or PCR testing: More sensitive but not widely available in dogs.
🛠️ Treatment Options
📌 First-Line Anthelmintics
- Fenbendazole: Typically 50 mg/kg PO daily for 5–10 days; success may vary.
- Ivermectin (off-label): Often given weekly for several weeks (e.g., fortnightly ×12 doses) and effective even when fenbendazole fails.
- Macrocyclic lactones: Moxidectin, milbemycin, also appear effective.
🔁 Managing Autoinfection
- Repeated dosing every 2 weeks until two consecutive negative Baermann tests.
- Monitor for relapse for several months post-treatment.
🔬 Supportive Care
- Fluids and electrolytes for diarrhea-related dehydration.
- Antibiotics if secondary bacterial enteritis is suspected.
- Corticosteroids for severe respiratory or dermatologic inflammation—use carefully to avoid exacerbating autoinfection.
- Nutrition support to address weight loss and malabsorption.
📈 Prognosis & Monitoring
- Mild cases respond well to anthelmintic therapy.
- Young or immunocompromised dogs require prolonged treatment and close monitoring; hyperinfection carries higher mortality risk.
- Recheck every 2 weeks during treatment and monthly for 3–6 months post-clearance.
- Prevent reinfection by maintaining hygiene—proper feces cleanup, kennel sanitation, and preventing soil contact.
🏡 Prevention Strategies
- Ensure clean housing with low humidity; avoid moist, contaminated soil.
- Regular deworming using broad-spectrum protocols; include fenbendazole or macrocyclic lactones in endemic areas.
- Promptly remove feces and disinfect kennel floors (heat, steam, etc.).
- Restrict access to areas with potential human-animal fecal contact to minimize zoonotic exchange.
📱 Ask A Vet Telehealth Support
- 📸 Upload stool, skin, and cough videos for remote assessment and triage.
- 🔔 Receive reminders for multiple treatment rounds and re-testing schedules.
- 🧾 Get guidance on sample collection for Baermann testing.
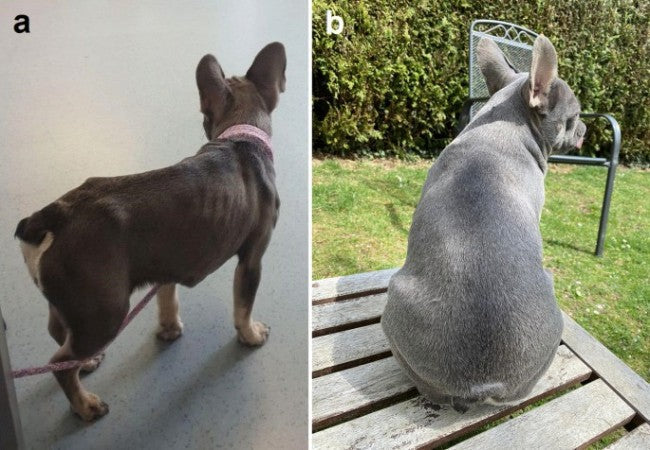
🎓 Case Spotlight: “Bella” the Stray Pup
Bella, a 3-month-old rescue pup from a humid shelter, presented with chronic diarrhea, weight loss, and occasional coughing. Baermann test confirmed Strongyloides L1 larvae. A 10-day fenbendazole course improved diarrhea initially, but larvae persisted. Weekly ivermectin for six weeks cleared the infection, confirmed by serial testing. Ask A Vet helped coordinate medication schedule, stool sample collection reminders, and nutritional support. Bella recovered fully and gained weight with stable GI function. 🌟
🔚 Key Takeaways
- Strongyloidiasis is an often silent but potentially severe nematode infection in dogs—watch for diarrhea, cough, dermatitis.
- Riskier in young, immunocompromised, or poorly housed dogs.
- Diagnose with Baermann fecal tests and repeat serially.
- Treat with fenbendazole or ivermectin—repeat doses required to halt autoinfection.
- Prevent through hygiene, deworming, and environmental care.
- Ask A Vet telehealth offers remote diagnostics, treatment reminders, medication delivery, and recovery guidance. 🐾📲
Dr Duncan Houston BVSc, founder of Ask A Vet. Download the Ask A Vet app today to manage strongyloidiasis—stool sample reminders, treatment monitoring, tele-triage, and home care for your dog 🐶📲






